All Program Year 2016 applications must be submitted by midnight, March 31st, 2017!
Last Year to BEGIN the Medicaid EHRIP
Eligible providers can receive incentive payments for up to six years, but Program Year 2016 will be the last year for providers to begin the Medicaid EHRIP.
The deadline to meet the eligibility requirements is December 31, 2016. Providers will have until March 31, 2017 to register with CMS and to submit their applications to the Vermont Medicaid EHRIP.
Get Started
First-time participants starting the Mediciad EHR Incentive Program in 2016 can follow the guidance listed here to understand how to begin, and how to meet program requirements for ongoing participation.
There are four steps to getting started:
- Review the basics
- Determine eligibility
- Register with CMS
- Align the information at CMS with the Vermont Medicaid data system.
Once registered with and determined eligible by both CMS and Vermont Medicaid, a provider has a maximum number of six years to engage in the program requirements and receive a yearly payment. CMS has indicated that new, first-time participants will be able to register at the CMS Registratrion & Attestation (R&A) site through the end of March 2017. PLEASE NOTE that the process to register at the R&A site and have the information available to attest takes several days complete, so providers cannot wait until 3/31/17 to register or they will miss the attestation deadline.
First Year A/I/U, then Five Years of Meeting Meaningful Use
Each provider who has been deemed an Eligible Professional (EP) must demonstrate patient volume thresholds for each year of program participation in order to receive a Medicaid EHR incentive payment.
Adopt/Implement/Upgrade
For the first year of participation, an EP may demonstrate that they have Adopted, Implemented or Upgraded (commonly abbreviated as A/I/U) their Certified Electronic Health Record Technology, which is defined as follows:
Adopt: Acquiring, purchasing or securing access to certified EHR technology.
Implement: Installing or commencing utilization of certified EHR technology capable of meeting meaningful use requirements.
Upgrade: Expanding the available functionality of certified EHR technology capable of meeting meaningful use requirements at the practice site, including staffing, maintenance, and training, or upgrade from exiting EHR technology to certified EHR technology per the EHR certification criteria published by the Office of the national Coordinator of Health Information Technology (ONC).
To apply for an A/I/U payment, each EP must attest individually, or have someone attest on their behalf, that the requirements of eligibility, patient volume threshold, and A/I/U criteria have been met, as well as providing documentation for the acquisition of the CEHRT in the form of an invoice, license agreement or similar proof of ownership.
Meaningful Use
The potential benefits of Electronic Health Records depend on how they are used. Meaningful Use is the set of standards defined by CMS that governs the use of EHRs by setting specific criteria for eligible professionals.
Eligible Professionals (EPs) have the option of attesting to Meaningful Use (MU) in their first year of participation in the EHR Incentive Program, but they must meet Meaningful Use criteria in order to receive payments in participation years 2 - 6. CMS has published EP Specification Sheets for the Meaningful Use Objectives and Measures for Program Year 2016.
The first year an EP demonstrates Meaningful Use, the reporting period for meeting the MU Objectives and Measures is 90 days. CMS is also extending the option for all providers to ulitlize a 90-day EHR Reporting Period for Program Year 2016 and Program Year 2017.
CQMs
In addition to Meaningful Use Objectives, each provider will attest to a set of Clinical Quality Measures (CQMs). The latest edition issued by CMS are the 2014 CQMs, which are still operative for EHR Incentive Program applications for 2016.
- Electronic submission of CQMs (eCQMs) is NOT required for the Vermont Medicaid EHRIP in Program Year 2016.
- EPs choose and report on nine of a possible list of 64 CQMs, and they must cover three of six National Quality Strategy domains.
- The CMS EHRIP website has a resource page describing requirements and tips for 2014 CQMs.
To apply for a Meaningful Use payment, each EP must attest individually, or have someone attest on their behalf, that the requirements of eligibility, patient volume threshold, and MU criteria have been met, as well as providing documentation to include EHR reports produced from the CEHRT, to include MU Objectives and CQMs, and other ancillary evidence of complying with various MU Objectives and Measures.
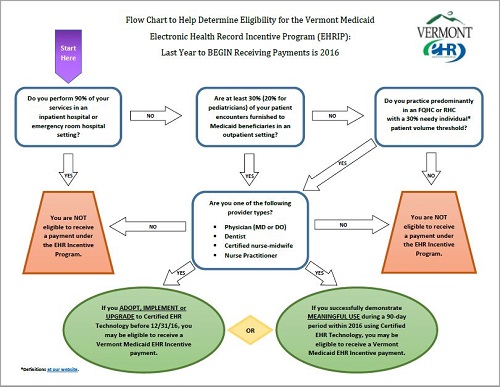
Eligibility Flowchart and Maximum Payment Chart
Click on the image below to open a larger version of the Eligibility Flow Chart to determine your ability to participate in the EHR Incentive Program.
Maximum EHR Incentive Payments for a Provider Beginning in Calendar Year (CY) 2016

Register with CMS
The Centers for Medicare & Medicaid Services developed this Checklist so that providers can gather the information needed before accessing the Registration and Attestation (R&A) system. Actions you may need to take:
- Ensure you have an active and approved enrollment record in the Provider Enrollment, Chain and Ownership System (PECOS).
- Confirm your Payee selection and email address.
- Designate an individual to attest on one or more providers' behalf, and ensure the provider's NPI, the Payee TIN and Payee NPI is accurate.
- Designate an entity to receive a payment on the provider's behalf.
- Obtain or confirm the EHR Certification Number -- also known as the CEHRT ID. Obtaining the CEHRT-ID on the ONC website can be confusing. A document stepping through the process, including screenshots, is available for download here. (Thanks to Cindy of the Pennsylvania EHRIP/MAPIR Team!)
Instructions and guidance on how to complete the above tasks are on the helpful CMS Checklist.
Success with First-time Registration Confirmed with a “Welcome” Email from MAPIR
Vermont is one of thirteen states using the Medical Assistance Provider Incentive Repository (MAPIR) System to manage Medicaid EHRIP applications. MAPIR (pronounced “mapper”) is the web-based state-level information system that tracks provider information regarding registration, attestation and EHRIP payments. Eligible Professionals participating in the EHR Incentive program will use MAPIR to submit their initial applications and annual attestations. MAPIR is accessed at the Provider Web Services Portal on the Vermont Medicaid website.
When Vermont’s MAPIR system has received and matched your provider information, you will receive an e-mail welcoming you to begin the MAPIR application process.
Receipt of the welcome e-mail may take several days from the time you complete your Federal registration, but it is confirmation that the necessary exchange of data between the R&A system and the Vermont Medicaid and MAPIR systems has occurred. You will not be able to proceed in MAPIR until this data exchange is successfully completed.
Once you receive your welcome email from MAPIR, you are on your way to completing your EHR Incentive payment application. An eligible provider -- or a preparer on their behalf -- will be able to log in to the secure Vermont Medicaid Provider Portal, follow the link to connect to MAPIR, and complete the following tasks:
- Confirm your CMS R&A information;
- Confirm or update the EHR Certification number (CEHRT ID) for your EHR system;
- Attest to your Medicaid patient volume, and
- Attest to your Meaningful Use criteria (if applicable);
- Upload the required documentation to support your EHRIP application
You can follow the guidance at our Vermont Medicaid EHRIP Application Process webpage which includes helpful links:
- Common MAPIR access troubleshooting tips;
- The EP MAPIR User Guides and
- The EHRIP Team and MAPIR Helpdesk.
EHR Incentive Program Audits
Audits of incentive payments are a required element of the EHR Incentive Program. Providers who receive an EHR incentive payment may be subject to an audit. The guidance provided in our Vermont Medicaid EHRIP Audit Tip Sheet will help ensure all the information required is submitted at the time of attestation, which is the best time to prepare for a potential audit.
For questions, contact the Vermont EHRIP Team at ahs.dvhaEHRIP@vermont.gov
Back to the Vermont Medicaid EHRIP Home Page
(Page last updated 1/24/2016)