The MAPIR User Guides for Program Year 2020 are available HERE.
- 2015 CEHRT Edition Required
- MU and CQM Reporting Periods
- Multiple Locations/Employers
- MU Stage 3
- Public Health Reporting for MU3
- Clinical Quality Measures
- Actions Allowable Outside the 90-Day EHR Reporting Period
- Updated Guidance on Objective 7, Health Information Exchange
2015 Edition CEHRT Required
You MUST be using a 2015 Edition Certified EHR System. The EHR system 2015 Edition CEHRT ID will contain “15E” in the third through fifth digits. Consult your EHR vendor if you are unsure of the certification standard of your system.
For your Meaningful Use (Promoting Interoperability) Reporting Period, you must be using a 2015 Edition CEHRT for the entire 90-day reporting period.
MU and CQM Reporting Periods in PY2020
- The EHR/MU Reporting Period is 90 days in 2020 for all providers.
- The Clinical Quality Measure reporting period is 90 days in 2020 for all providers.
Multiple Locations/Employers
Those preparing and submitting applications for incentive payments in the Medicaid Promoting Interoperability Program MUST be cognizant of whether the providers they are preparing applications for practice at other locations or have other employers.
We recommend that preparers flag any provider who either:
- Practices at another location (in most instances when it is the same employer that has multiple practice sites, the CEHRT automatically combines the data, so there will likely be no extra steps needed),
OR
- Has more than one employer.
For each of these providers, you should confirm that at least 50% of their total outpatient encounters during their EHR reporting period took place at a location, or a combination of locations, with certified EHR technology (CEHRT).
Meaningful use measures can be calculated across locations and employers by adding the numerators and denominators from each CEHRT.
Please be advised that you will be putting your organization at risk of recoupment during post-payment audit if you do not consider all of the locations and employers of your attesting Providers. Furthermore, please be aware of the dates you are entering in your applications. The EHR Reporting Period should be used when completing the MU General Requirements section of the MAPIR attestation, not the Patient Volume dates.
Please refer to CMS guidance on multiple locations for further information: Guide for Eligible Professionals in the Medicaid Promoting Interoperability Program Practicing in Multiple Locations.
MU Stage 3 Objectives and Measures
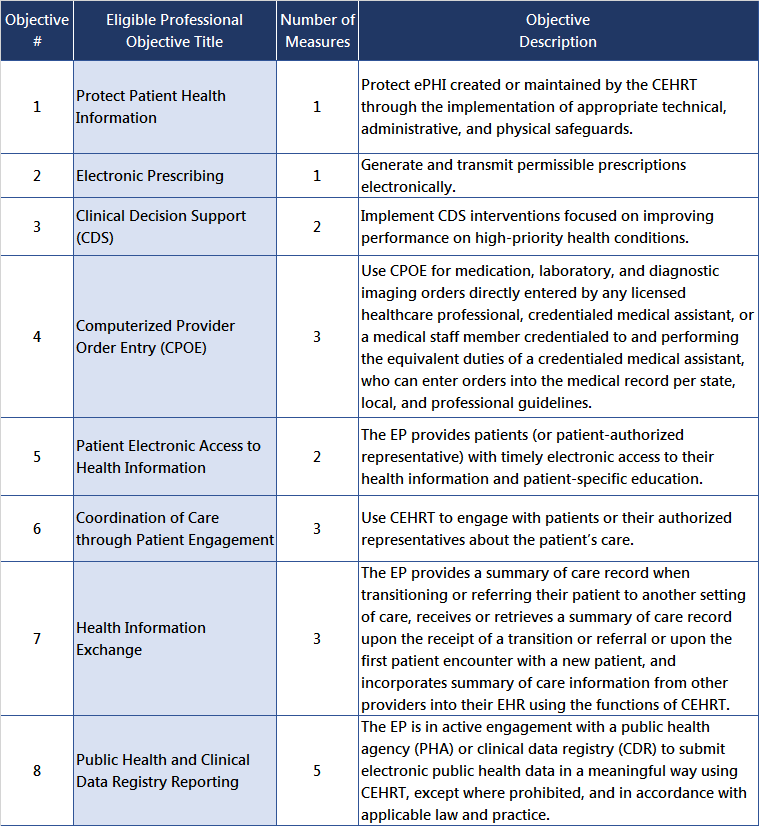
Meanginful Use Stage 3 requirements have been reorganized into eight Objectives with a total of 20 Measures. The CMS Specification Sheets for the 2020 Medicaid Promoting Interoperability/EHR Incentive Program are posted at the CMS PY2020 webpage.
Public Health Reporting Objective in MU3
Important changes to the Public Health/Clinical Data Registry Reporting requirements (MU3 Objective 8) will affect how Eligible Professionals will select and complete the measures. Because Vermont and New Hampshire have different Public Health registries available, Vermont and New Hampshire EPs will have different requirements for attesting to Active Engagement or for taking an Exclusion to the meaures. Clink the link below for the guidance and Documentation Aids for the five Public Health Reporting/Clinical Data Reporting:
PY2020 MU3 Public Health Reporting Objectives
Clinical Quality Measures for Program Year 2020
All Clinical Quality Measures in the PIP/EHR Incentive Program are referred to as "eCQMS" because they must be generated by a provider's Certified Electronic Health Record system. EPs participating in the Vermont Medicaid PIP/EHRIP are not required to submit eCQMs electronically. Click here for additional guidance: PY2020 eCQM Reporting in MAPIR (PDF, 612 KB, Updated 7/10/2020)
Examples of the MAPIR screens for PY2020 eCQM data entry are available here:
CQM_Screenshots_PY2020_MAPIR_6.3 (PDF, 2.4 MB, Updated 7/10/2020)
The CMS Promoting Interoperability website posted updates for Clinical Quality Measure reporting for Program Year 2020:
Medicare Promoting Interoperability Program Requirements for 2020
Actions Allowable Outside the 90-Day EHR Reporting Period
Meaningful Use Stage 3 Objectives include measures for which action can occur before, during or after the MU reporting period of 90 days, but within the calendar year of each Program Year. Including data from the entire calendar year helps providers meet the thresholds for these measures. Each objective’s specification sheet lists the information under the ‘Additional Information’ section of any objective that allows this. In order to provide the necessary documentation to support inclusion of the data, the PIP/EHRIP Team requests a data file that verifies that the action that occurred outside the EHR Reporting period during the calendar year is valid for a patient seen during the 90-day EHR reporting period. More information can be found in this tipsheet:
ActionsAllowableOutside90DayReportingPeriod.pdf
Updated Guidance for MU3 Objective 7: Health Information Exchange
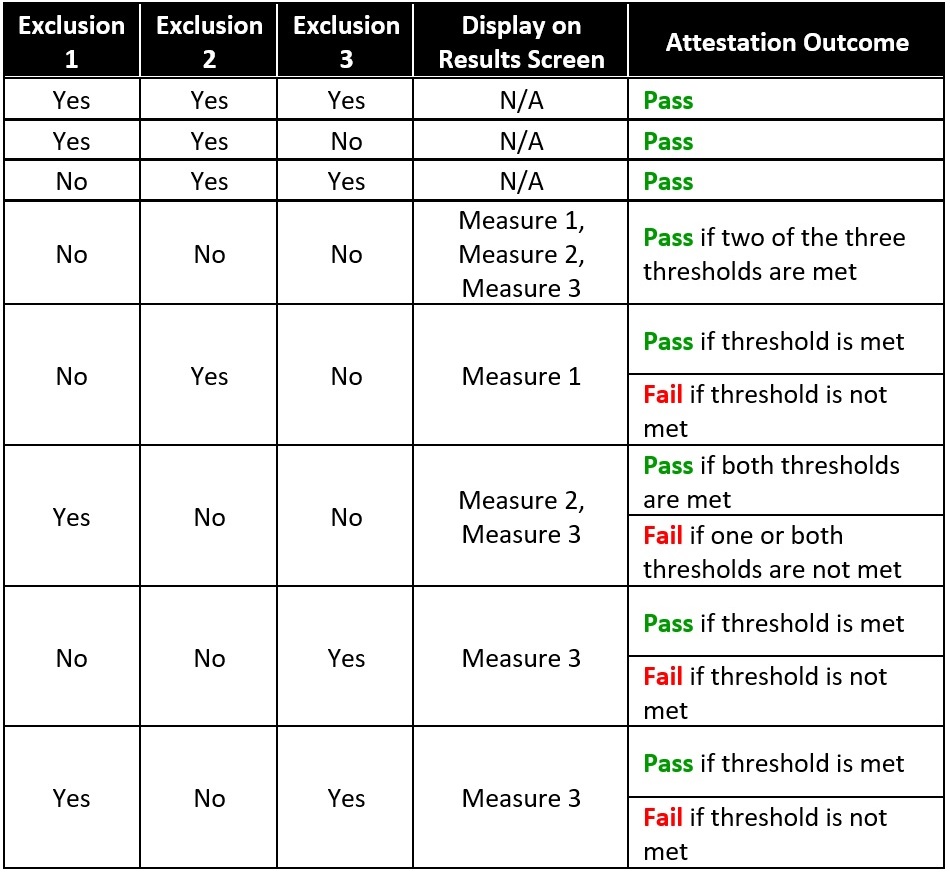
In July, CMS updated specification sheets with new criteria for EP Objective 6 and Objective 7 Meaningful Use attestation for Program Year 2019 and beyond. No modifications were required for the way MAPIR evaluates Objective 6, but the update did indicate a change for MAPIR pass/fail logic for Objective 7, Health Information Exchange, as follows:
- The objective will pass when two exclusions are taken and the threshold for the remaining measure is met.
- The objective will fail when an exclusion is selected for one measure, the threshold is met on a second measure, and the threshold is not met for a third measure.
This table displays the pass/fail outcomes of all the possible responses for Objective 7:
For questions, contact the Vermont EHRIP Team at ahs.dvhaEHRIP@vermont.gov
Back to the Vermont Medicaid PIP/EHRIP Home Page
(Page last updated 07/21/2020)